“Ana-Maria has been a blessing. We first met when I was in a very dark place, and she was there when I needed someone. She is professional and thorough and has gone above and beyond for me on many occasions. Ana is dedicated to her clients, and she genuinely cares. She is a credit to your organization.” ~ R.G. (client)

As the pandemic continued into 2021-2022, we continued offering many of our services virtually to support the people who needed them most. Our virtual access and call center phone system improved our connections to people, as our volume has grown further. Our crisis response services served 19,772 people, up 16% from last year, and another 34% from two years ago. That is a 56% increase in two years! This huge increase further highlights the need for support, revealing the impact the pandemic and recent global events have had on our communities.
We were thrilled to receive additional funding to open and operate four safe beds, specifically for people who encounter our police partners and need support. Our new program is set to launch in July 2022.
YSSN is proud to be participating partners with various Ontario Health Teams including Western York Region OHT, South Simcoe OHT, and a supporting partner of Southlake Regional Health Centre. Streamlined Access services have expanded with the Eastern York North Durham OHT to provide a direct referral pathway for primary care physicians for mental health and addictions patients. The referral pathway is rolling out to primary care providers currently, with full onboarding in late 2022.
We are extremely grateful for having caring, dedicated staff who continue to serve the community on the front lines.
~ Jean West, Director of Mental Health, YSSN

Crisis has averaged an 11% growth rate in calls and visits over the past 4 years. Through our crisis response services, we served 19,772 people, up 15% from last year (and up 56% from two years ago), with 30,461 contacts/visits.
Crisis



Safe beds
YSSN received base funding to operate four safe beds in York Region (three in Richmond Hill, one in Newmarket). These beds are available specifically for police and Mobile Crisis Response Teams (MCRT). They will be available to all our police partners. The beds will support individuals who encounter police, who are not appropriate for hospital or jail, but need support. Stays will be up to 30 days. Staff are on-site and will provide 12-hour support, seven days a week. Support will range from crisis intervention, de-escalation and stabilization, support with ADL’s, connection to resources, and follow-up. This program is set to launch in July 2022.

Mental Health Support Team
Our Mental Health Support Team (MHST) crisis workers saw an increase of 24% in requests for service. Whether driving through winter blizzards and slippery roads, to risking their own health to work face-to-face throughout a global pandemic, our MHST crisis workers have shown commitment, passion, empathy, and flexibility, each and everyday. They’ve been working on the frontlines in our communities, responding to calls that have increased in both volume and complexities. The team has truly embodied the spirit of YSSN by being, bold and nimble, thriving and acting on change, and truly taking a lead on ensuring positive outcomes in a adapting and complex ecosystem.





Ontario Health Teams
We continue to value our partnerships with various Ontario Health Teams, including East York Region North Durham Ontario OHT, Western York Region OHT, South Simcoe OHT, and Southlake OHT. We are working with EYRND-OHT to expand Streamlined Access services to primary care physicians.
Since 2007, Streamlined Access has expanded to become the access mechanism to the Assertive Community Treatment Teams, Psychogeriatric Assertive Community Treatment Teams, and Mental Health and Addictions Supportive Housing. Most recently, Streamlined Access has developed referral pathways specifically for two initiatives: primary care providers EYRND OHT and the Youth Transitions and Navigation project across Regional OHTs in York Region.
The purpose of the primary care referral pathway is to connect patients to community mental health and addictions services, through Streamlined Access. The referral pathway was launched to a small number of primary care providers in EYRND OHT in July 2021 with full onboarding in the winter of 2022. To support primary care providers, Streamlined Access will complete intake assessments, waitlist management for the 26 (and growing) programs offered through Streamlined Access, offer both peer and family caregiver support, and navigation to services that are not available through Streamlined Access.
Streamlined Access services have expanded with the Eastern York North Durham OHT to provide a direct referral pathway for primary care physicians for mental health and addictions patients. The referral pathway is rolling out to primary care providers currently, with full onboarding in the winter of 2022.
The Youth MHA Navigation and Transition program is a collaboration of youth mental health agencies and addiction service community partners and hospitals in York Region (York Hills, Reena, 360 Kids, Your Support Services Network, Southlake Regional Health Centre, Oak Valley Health and Mackenzie Health). This initiative is focused on Regional Ontario Health Teams in York Region, patients, and caregivers with the goal of improving patient experiences by designing seamless transitional care pathways for youth ages 16-28 with mental health conditions and addictions to Streamlined Access.

Partnerships
We continue to provide some virtual mobile response through Kinark, York Region. In April 2021, we expanded our After Hours service to youth/families via telephone, text and live chat. We continue to take calls and make referrals for individuals living in other regions as well including Durham, Kawartha Lakes, Peterborough, and Haliburton.
EMS referrals and follow ups continue to come in on a regular basis. Many community agencies continue to reach out to us and us to them; we see the value in sharing our programming strategies and management around COVID and supporting clients who have been impacted by so many issues, including homelessness.

The Call Diversion Unit (CDU) was asked by the Criminal Investigations Bureau to follow up with an individual. During the call, the individual shared that she moved to York Region in Spring of 2020 and was not connected to any services here. She used to receive services, including a psychiatrist and a case manager, in the previous community she lived. I provided orientation to Streamlined Access and the individual provided consent to do the referral; the referral was completed at the time of call.
I followed up with Streamlined Access this week. There assessment was completed, and the individual went on the waitlist for case management services. This is an example of where a police contact brought community supports to the individual.
~ YSSN Staff
We connected 8,686 people to access services, up 15% from the previous year. Of those, we linked 3,414 people to mental health, addictions, dual diagnosis, and housing supportive services through Streamlined Access. We answered 5,178 inquiries and received 1,951 referrals. We saw a total increase of 24% in Mental Health Support Team calls and visits from last year.
We answered 26,007 inquiries and served 5,272 people through Developmental Services Ontario Central East Region to help families and adults with developmental disabilities access information and resources to help them navigate service systems. We completed 1,134 applications and 952 intakes for adults with developmental disabilities who were eligible for funded services.

Through our crisis response services, we served 19,772 people, up 15% from last year (and up 49% from two years ago), with 30,461 contacts/visits.
We linked 3,414 people to mental health, addictions, dual diagnosis, and housing supportive services through Streamlined Access. We answered 5,178 inquiries and received 1,951 referrals.


“A female with a diagnosis of bi-polar disorder had been experiencing chronic instability in housing after a fire damaged her apartment. The youth reported being homeless for the past three years; sleeping in tents, trailers, and a re-occurring visitor at multiple hospitals. She had been attempting to received mental health support for the past few years, unsuccessfully, and reports using self-harm behaviours including substance abuse as a coping mechanism.
The youth was referred to the Transitional Aged Youth program where she connected with a Transitional Aged Youth Navigator at Streamlined Access. The Navigator listened to her story, triaged her needs, and connected her to resources that would support her in the short and long term. The youth was also connected to a Case Manager who will support her with her mental health symptoms and substance use and develop positive coping strategies. The Case Manager will also support her in finding stable housing, and with any other needs as they arise. The youth was also connected to a trauma therapist to support working through her trauma through a trauma-informed lens. The youth will now be able to connect with the Transitional Aged Youth Navigator, at any time, should her needs change or she require additional support. When she ages out of the Transitional Aged Youth program, she will receive the same level of support from Streamlined Access, throughout her adult life.”
~ YSSN Staff
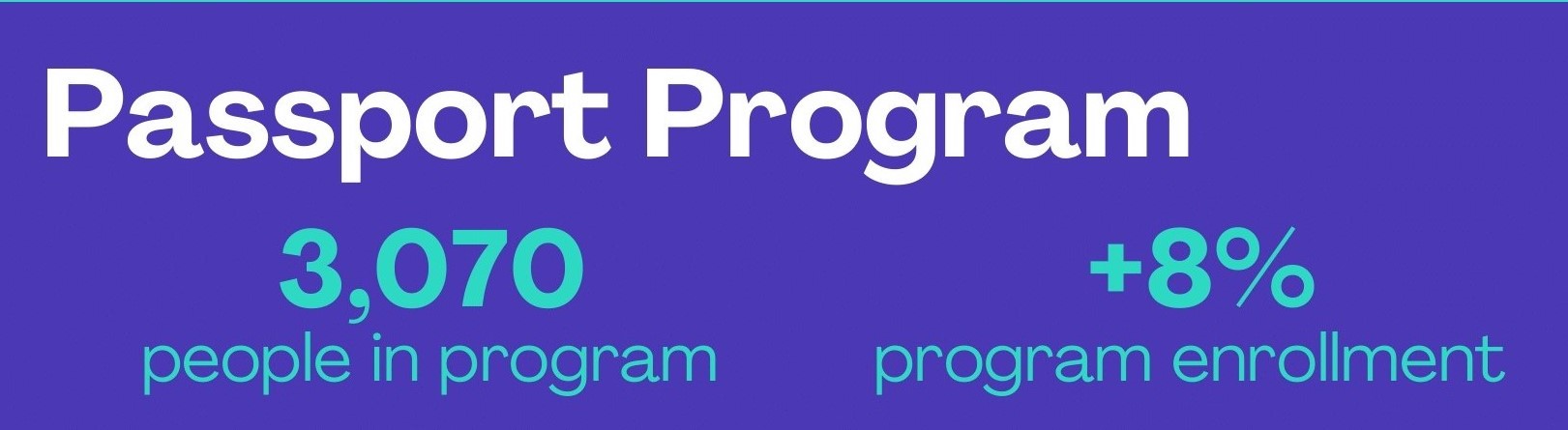
We served 3,070 adults with a developmental disability through our Passport Program, an 8% increase in program enrollment compared to the previous year.
“TW is a 62-year-old male with a diagnosis of Schizophrenia and a history of complex needs and behaviours. He has lost housing multiple times and was homeless at time of referral and inpatient at hospital. When an Access worker reached out, he had been transferred to another hospital for a lengthy admission. Hospital staff contacted Streamlined Access months later as he was being discharged without housing and would be staying temporarily with a family member out of the region. The Access worker spent considerable time connecting with staff at several hospitals, family members and the client himself. The client secured housing at a hostel and intake was completed for PACTT. The client and family were very pleased that Flex support was arranged in the meantime as PACTT waitlist is so lengthy. In addition, his family member was offered Family Navigation support which she is considering.”
~ YSSN Staff


“JR is a referral from one of our Primary Care Physician partners. While he reported receiving mental health care in his youth, he remained stable for many years, but noticed a decline early in the pandemic. This was intensified by job loss, the declining health of one of his parents, and the end of a long-term relationship. Due to these challenges, he was in between homes, which took him approximately two years to address, only having some resolution around the time of assessment. However, it still acted as a barrier, as when he was attempting to access regional mental health services, he would not be eligible due to conflicting information regarding his addresses. This was very discouraging for JR, but also exacerbated by his anxiety and depression symptoms, which caused him to be fearful and overwhelmed, acting as a further barrier.
As a Streamlined Access Navigator, I worked with JR over multiple weeks to address the barriers he was facing. This included logistical barriers with his address; barriers from his symptoms; and the barrier of self-stigma. After three appointments with JR, we were able to navigate to appropriate services. JR noted that he also already noticed improvement in his mood from having someone to share his story with and discuss positive coping strategies.”
~ YSSN Staff
